Do you know what signs to look for to consider Neocate first? When a baby with food allergies needs formula, they need a formula that won’t trigger an allergic response. Hypoallergenic formulas are tailor-made for infants with food allergies. A hypoallergenic formula provides protein equivalents from either peptides (extensively hydrolyzed milk protein, to be exact1) or from non-allergenic amino acids.2
But extensively hydrolyzed formulas (eHF) and amino acid-based formulas (AAF) aren’t the same. An eHF manages symptoms for most infants with CMA (at least 90% of uncomplicated cases3,4), whereas AAFs are usually used for more severe cases or after an eHF “fails” to fully improve symptoms. But food allergies pose significant burdens and diagnosis can be delayed.5 It’s no wonder many caregivers want to see symptoms managed quickly and often ask you for the surest option first. Sometimes, the evidence and guidelines support choosing an AAF first-line.
Let’s review potential signs you could look at to determine if a hypoallergenic amino acid-based formula, like Neocate, can be considered and recommended over an eHF to manage cow milk allergy.
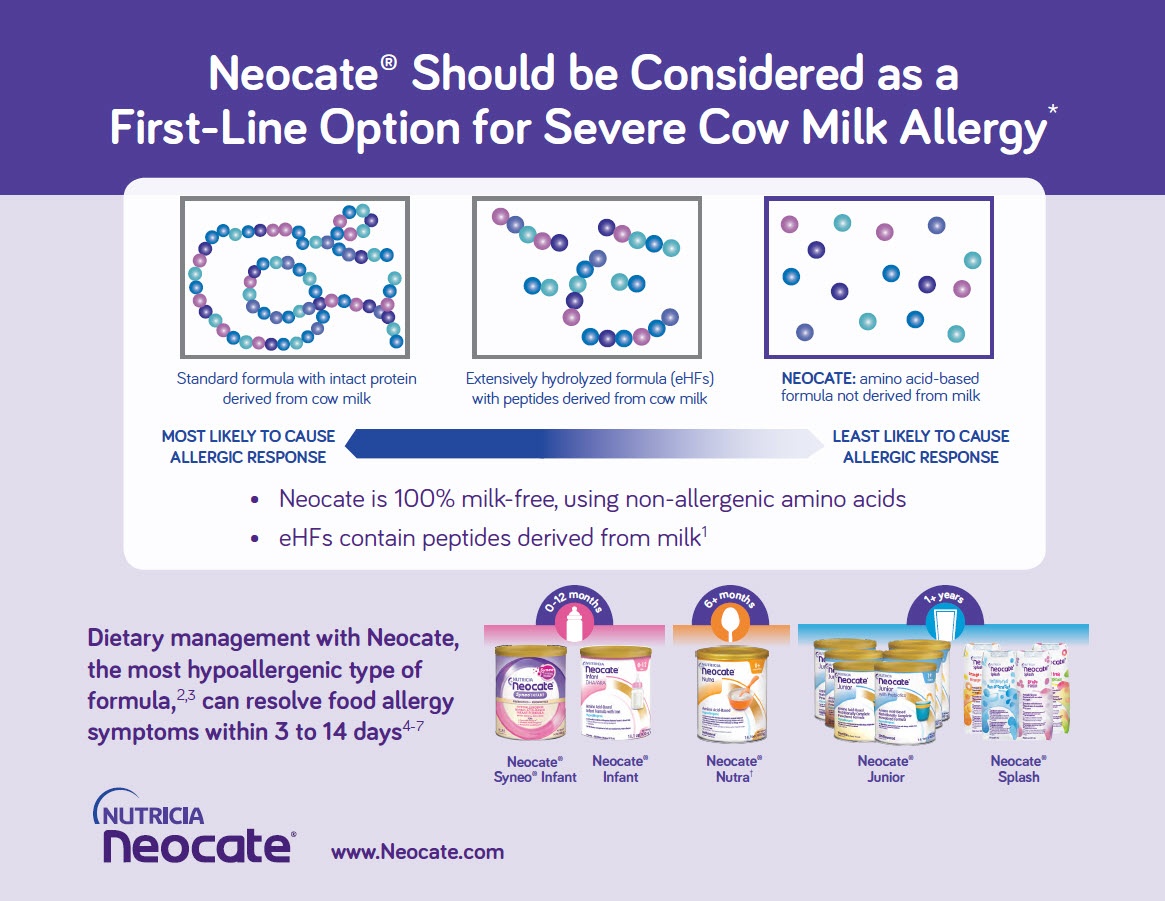
Available Types of Baby Formula
First, let’s review available types of baby formulas in the below table. Infant formulas vary by the kind of protein used to make them and the size of the protein. The source and size of protein determine how allergenic – or likely to trigger an allergic reaction – a formula is for patients with cow milk allergy (CMA).
| Protein Structures in Formulas | Source of Protein | Protein Type / Form | Allergic Reaction Potential |
Whole protein Cow/Soy milk protein |
Cow Milk Goat Milk |
Whole Protein Casein or Whey |
Most Allergenic Least Allergenic |
| Soy Milk | Whole soy protein & soy isolate | ||
|
Peptides (hydrolyzed protein) |
Partially or Extensively Hydrolyzed | Fragments of cow milk protein Casein hydrolysates or Whey hydrolysates |
|
Amino acids Not derived from dairy or soy |
NEOCATE |
100% Amino acids |
The signs and symptoms of a cow milk allergy can vary, and an infant with food allergies often shows more than one. You use your clinical judgment when deciding which formula to recommend. And sometimes the patient must meet criteria to qualify for specialty formula coverage. But if you see patients with cow milk allergy less often, here are the scenarios for which evidence strongly supports considering an amino acid-based formula like Neocate first.
Red Flag Indicators to Consider Neocate First for Cow Milk Allergy Management
-
Symptoms Not Resolved on an Extensively Hydrolyzed Formula (eHF)3,6-9

Healthcare professionals often refer to medical guidelines for managing food allergies. Guidelines generally recommend an eHF first to manage CMA. At least 90% of infants with CMA should tolerate an eHF,3,4 although this could be as low as 60% among infants with more severe CMA.4 If food allergy symptoms don’t completely resolve within 2-4 weeks on an eHF, international guidelines recommend an AAF like Neocate should be used next instead of a different eHF.3,7 The reason? If one eHF fails to fully resolve symptoms, another eHF is not likely to be better.
-
Poor growth, especially with multiple food eliminations and/or GI tract/skin symptoms7-9
 Children whose severe food allergies aren’t under control may have poor growth. For these children, poor growth can overlap with other conditions.
Children whose severe food allergies aren’t under control may have poor growth. For these children, poor growth can overlap with other conditions.
When poor growth shows up with GI tract and/or skin symptoms, the evidence supports choosing an AAF, like Neocate, over an eHF.9 That’s because skin symptoms can signal inflammation that can increase nutrient needs, leading to poor growth. And gastroesophageal reflux related to severe CMA may be associated with poor weight gain and unresponsive to management.6,7
Another combination – poor growth plus multiple food allergies – can lead clinicians to consider an AAF like Neocate. That’s because infants with multiple proven food allergies often have more severe cases.9 And infants who must avoid 3 or more foods due to allergies have been found to have worse growth parameters and nutritional intake.9,10
-
Severe Gastrointestinal (GI) Allergies3,7-9,11
 Many cow milk allergy signs and symptoms relate to the GI tract. Allergic conditions that affect the GI system can be severe and might indicate the need for a hypoallergenic AAF like Neocate.9,12 While “severe” isn’t clearly defined, blood in the stool that doesn’t respond to management can signal a severe GI allergy.8,13
Many cow milk allergy signs and symptoms relate to the GI tract. Allergic conditions that affect the GI system can be severe and might indicate the need for a hypoallergenic AAF like Neocate.9,12 While “severe” isn’t clearly defined, blood in the stool that doesn’t respond to management can signal a severe GI allergy.8,13
Specific conditions healthcare teams might look for when considering hypoallergenic formula options include food protein-induced enterocolitis syndrome (FPIES) and eosinophilic esophagitis (EoE). These can come with severe GI symptoms, like vomiting or reflux, and cow milk allergy is often part of these conditions.14-16 For managing EoE with diet, an AAF should be used when formula is needed.9,11 In fact, symptom resolution and histological remission on AAF has been shown to be more than 90% in children and adults with EoE.9,17,18 For FPIES, an AAF is preferred over an eHF when FPIES occurs in combination with poor growth.7,19
-
Anaphylaxis9,11
Anaphylactic reactions to food allergens can be severe and life-threatening, and acute reactions to cow milk occur in between 0.8%-9% of CMA cases.9,11 In patients who have had anaphylaxis to cow milk, consensus guidelines from an international panel recommend a hypoallergenic amino acid-based formula, like Neocate.9,11
Other Factors the Medical Team Might Consider
The signs and symptoms of CMA vary. Some have not been studied as much as others, meaning evidence for which formula type to use first in some scenarios or conditions is less clear. These often overlap with other symptoms. In those cases, guidelines advise an eHF is usually the first choice. Here are some additional symptoms that healthcare teams might consider when deciding which type of hypoallergenic formula to use.
Severe Eczema4,7
Some patients have both eczema, or atopic dermatitis, and food allergies.7,20 In fact, roughly one-third of children with moderate-to-severe eczema also develop food allergies. It can be hard to link eczema to specific food triggers because eczema flares can be delayed, and inflamed tissues take time to heal.
Most medical guidelines recommend that either eHF or AAF be used for infants with cow milk allergy and eczema.11,21 Some suggest an amino acid-based formula like Neocate for infants with severe eczema when fed breast milk.3,7 However, until there’s better research, an eHF should be tried first for severe eczema.9 But as covered above, an AAF like Neocate should be considered first-line for infants with poor growth and severe eczema.7-9
Multiple Food Allergies
About 33% of cow milk allergy patients may develop allergies to other foods,22,23 and children with multiple food allergies (MFA) tend to have more severe cases.9 Like severe eczema, guidelines have suggested skipping extensively hydrolyzed formulas and going straight to AAF for these patients.3,21 However, this is based on limited science, so you should recommend an eHF first for infants with MFA alone.9 Note: An AAF like Neocate can be recommended first for infants who show both poor growth and multiple food allergies.7-9
Cow Milk Allergy Symptoms while Fed Breast Milk4,7,8
Breast milk is the preferred nutrition for infants,7 and Nutricia supports feeding breast milk wherever possible. In some cases, infants with cow milk allergy have developed symptoms to breast milk.1 Dairy protein in a lactating woman’s diet can lead to fragments of cow milk protein in her breast milk. These fragments can be similar in size to the peptides in eHFs.1,7,24
For infants who react to cow milk protein fragments in breast milk, you may advise the mother to eliminate dairy from her diet under medical supervision.3,7,8 For example, maternal elimination diets are typically required for proctocolitis, although not always needed. And with FPIES, the general advice is that maternal elimination is typically not required as FPIES is not commonly triggered by food peptides that pass into maternal milk.16
When formula is needed for these babies to supplement or replace breast milk, guidelines have suggested using an AAF like Neocate first,21 or either an eHF or AAF first,3,22 based on limited data. However, the evidence supports trying an eHF first.9 A formula like Neocate should be used if the baby doesn’t tolerate an eHF.
What to Expect When You Recommend Neocate
Neocate is the most hypoallergenic type of formula,20,25 and when used in the dietary management of food allergies it can resolve symptoms within 3 to 14 days.24,26-28
For infants with CMA, Neocate Syneo Infant is the first and only amino acid-based formula with pre- and probiotics designed to help support immune function. Read more about Neocate Syneo Infant and what makes it unique.
When you see an older child diagnosed with food allergies, you can recommend Neocate Splash, the first and only hypoallergenic amino acid-based formula that’s ready to drink. Read about great-tasting, convenient Neocate Splash.
Resources
|
A quick reference guide to the 4 red flag indicators when you can go straight to Neocate, supported by guidelines and research. |
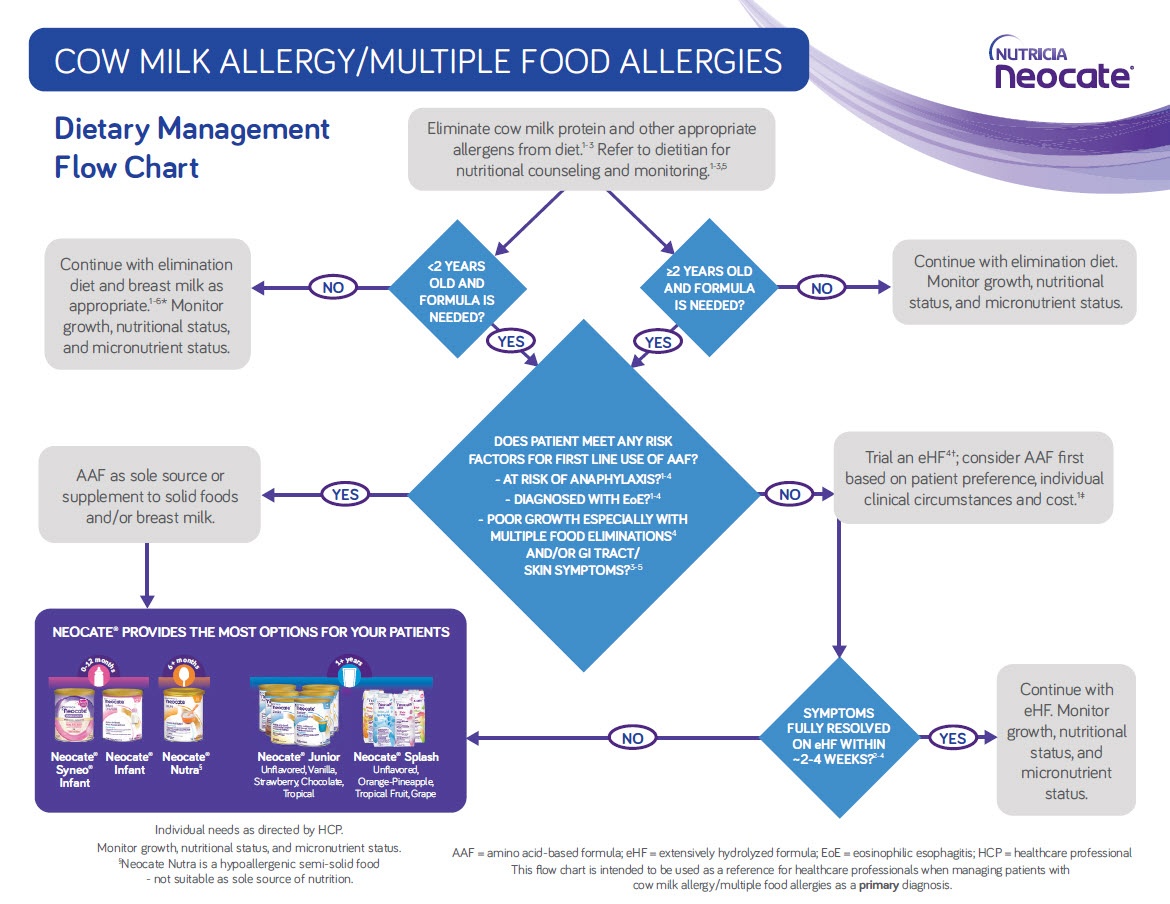
An evidence-based flowchart to help you with dietary management decisions for patients with cow milk allergy or multiple food allergies. The flow chart poses guiding questions and considerations to ensure patients’ nutrition needs are being met. It includes a list of the Neocate family of products. |
Watch an educational webinar with speakers Dr. Rosan Meyer and Dr. Carina Venter: When to Use Amino Acid-based Formula to Manage Cow Milk Allergy. |
Read a thorough review of the evidence: When Should Infants with Cow’s Milk Protein Allergy Use an Amino Acid Formula? A Practical Guide.
 Rob McCandlish, RDN
Rob McCandlish, RDN
Rob is a registered dietitian nutritionist (RDN) who joined Nutricia in 2010. He has spent years talking with Neocate families, working with practicing clinicians, and learning about the science behind Neocate and food allergy research. Rob has two nephews who both used Neocate for their cow milk allergies!
- Host, et al. Allergy. 2004;59 Suppl 78:45-52.
- Pediatrics. Pediatrics. 2000;106:346-49.
- Koletzko, et al. J Pediatr Gastroenterol Nutr. 2012;55:221-9.
- Hill, et al. Clin Exp Allergy. 2007;37:808-22.
- Lozinsky, et al. Children (Basel). 2015;2:317-29.
- Vandenplas, et al. Arch Dis Child. 2007;92:902-8.
- Venter, et al. Clin Transl Allergy. 2013;3:23.
- Ludman, et al. BMJ. 2013;347:f5424.
- Meyer, et al. J Allergy Clin Immunol Pract. 2018;6:383-99.
- Meyer, et al. J Hum Nutr Diet. 2014;27:227-35.
- Fiocchi, et al. Pediatr Allergy Immunol. 2010;21 Suppl 21:1-125.
- Latcham, et al. J Pediatr. 2003;143:39-47.
- Groetch, et al. J Allergy Clin Immunol Pract. 2013;1:323-31.
- Gonzalez-Cervera, et al. J Investig Allergol Clin Immunol. 2016;26:8-18; quiz 2p following
- Molina-Infante, et al. Expert Rev Gastroenterol Hepatol. 2017;11:115-23.
- Nowak-Wegrzyn, et al. J Allergy Clin Immunol. 2017;139:1111-26.e4.
- Groetch, et al. J Allergy Clin Immunol Pract. 2017;5:312-24.e29.
- Liacouras, et al. Clin Gastroenterol Hepatol. 2005;3:1198-206.
- Motala, et al. http://www.worldallergy.org/professional/allergic_diseases_center/cows_milk_allergy_in_children/ [March 6, 2019].
- du Toit, et al. Arch Dis Child Educ Pract Ed. 2010;95:134-44.
- Luyt, et al. Clin Exp Allergy. 2014;44:642-72.
- Boyce, et al. Nutr Res. 2011;31:61-75.
- Host, et al. J Allergy Clin Immunol. 1997;99:S490(1988).
- de Boissieu, et al. J Pediatr. 1997;131:744-7.
- Host, et al. Arch Dis Child. 1999;81:80-4.
- Hill, et al. J Pediatr. 1999;135:118-21.
- Heine, et al. J Allergy Clin Immunol. 2003;111:S102.
- Vanderhoof, et al. J Pediatr. 1997;131:741-4.