
More and more children are developing food allergies. Did you know, cow milk protein is the most common food allergen in early childhood? It’s even more prevalent in infancy than peanut allergy. In fact, more than 100,000 babies each year – 2-5% of infants – suffer from this allergy in the US. Cow milk allergy (CMA) can also be called milk protein allergy, milk protein intolerance or cow milk protein allergy (CMPA). Want even more acronyms? Infants allergic to both milk and soy: milk soy protein intolerance (MSPI) or multiple food allergies (MFA). With such prevalence, do you know the common signs and symptoms of a cow milk allergy?
Children with a cow milk allergy often experience several signs and symptoms. These can affect multiple body parts, or systems (digestive, skin, respiratory or general). These are not specific to CMA, meaning they can signal other conditions. That makes CMA difficult to identify. First you must identify the cause of these signs and symptoms, then you can manage the condition and symptoms.
Parents often tell us they waited months before their child was officially diagnosed with CMA. This often involves multiple doctor visits with few answers. Being able to spot possible signs of CMA may lead to recognizing it earlier. That can mean quicker solutions, often a hypoallergenic amino acid-based formula like Neocate®.
When to Ask if Your Baby Might Have a Cow Milk Allergy?
The following video outlines 8 signs and symptoms that may cause a healthcare team to suspect CMA. The list comes from a Board-certified pediatric allergist.
This is certainly not a comprehensive list – some signs and symptoms are less common. Also, not every infant with one or more of these signs will be diagnosed with CMA. Finally, every infant who develops an allergy will have a unique experience.
Now, let’s dive a bit deeper into eight common signs of a cow milk allergy. Parents who see these in their baby can ask the doctor if they might signal CMA.
Digestive: Persistent Diarrhea or Constipation
Diarrhea can be very concerning to someone caring for an infant. Every infant has loose stools from time to time. However, if you see multiple loose or liquid stools a day, it could signal a milk allergy. (“Multiple” = average of 2-4 times a day for more than 5-7 days.) Over half of children with CMA can have diarrhea, the most common digestive symptom.
Remember: diarrhea has many causes. Ask your healthcare team if you think your little one has diarrhea. Here are great resources with more detail about baby bowel movements:
- Diarrhea and its link to CMA
- What is normal and what is not when it comes to baby poop
- What color should baby poop be?
Believe it or not, constipation can also signal CMA in infants. While constipation is a less common sign than diarrhea, it’s possible for infants with CMA to have constipation.
Digestive: Blood and/or Mucus in the Stool
Blood in the stool is a likely sign of CMA in infants. The blood results from inflammation in the gut. It can appear in the diaper as either red or black. Red blood means the bleeding is in the lower end of the gut. Black color usually signals bleeding higher up, like from uncontrolled reflux. If you notice red or black in your baby’s diaper, call the doctor.
Mucus looks like what comes out of your nose when you have a cold or runny nose. It looks sticky when you open the diaper. A little bit can be normal, but if you see a lot or it lasts a while, it can signal a food allergy.
Digestive: Frequent Vomiting, Reflux or Spitting Up
 Babies often spit up (or “regurgitate”), but anything beyond the occasional post-meal spit-up should be examined by a doctor. Many infants who spit up don’t seem bothered by it and maintain a healthy weight – we call them “happy spitters.” For other infants, spitting up may represent something more concerning like gastroesophageal reflux disease (GERD) or vomiting. It can lead to low or no weight gain.
Babies often spit up (or “regurgitate”), but anything beyond the occasional post-meal spit-up should be examined by a doctor. Many infants who spit up don’t seem bothered by it and maintain a healthy weight – we call them “happy spitters.” For other infants, spitting up may represent something more concerning like gastroesophageal reflux disease (GERD) or vomiting. It can lead to low or no weight gain.
In infants, frequent reflux or vomiting can be related to CMA. Almost 50% of infants with reflux may be diagnosed with CMA. In those cases, taking cow milk out of the diet should help relieve reflux. Read more information on reflux and vomiting in infancy. (In one extreme allergic condition –Food Protein Induced Enterocolitis (FPIES)– violent vomiting a few hours after feeding is the hallmark sign.)
Digestive: Persistent Gassiness
Gas happens when there is excess air in the stomach or intestines. This can result in discomfort, burping, or passing gas. Discomfort can cause an infant to be “fussy”, “cranky”, or “colicky.” All babies have gas, but when it occurs with several other signs, it signals a possible allergy to cow milk.
Skin: Unexplained Rash
 There are many causes for skin rashes, like atopic dermatitis (eczema) or hives (urticaria). CMA is a possible cause, especially when other CMA signs are present. Up to 70% of infants with CMA have skin-related signs. Rashes related to CMA may be very uncomfortable, with nonstop itching and scratching. This may be worse after feedings.
There are many causes for skin rashes, like atopic dermatitis (eczema) or hives (urticaria). CMA is a possible cause, especially when other CMA signs are present. Up to 70% of infants with CMA have skin-related signs. Rashes related to CMA may be very uncomfortable, with nonstop itching and scratching. This may be worse after feedings.
Rashes often appear on the face, but can appear anywhere on the body. Remember, it is important to check with your child’s physician if you suspect the rash to be related to CMA. For more information about skin rashes and when it might signal CMA, check out Baby Rashes from Acne to Eczema.
Respiratory Problems
Children can have different respiratory issues with CMA. Up to 30% of infants with CMA have respiratory signs. These generally fall into two types; either mild or severe.
- Mild–Includes runny noses, sneezing, and nasal congestion. These look like what you might see when your child has a cold.
- Severe–Includes shortness of breath, struggling to breathe or wheezing: all need immediate attention. Shortness of breath can look like sudden and/or severe gasping or difficulty breathing. Your child may look to be in pain and frightened. Wheezing is a whistling or rattling sound in the chest when a child breathes. Both indicate obstructed airways. If your child shows a severe respiratory symptom, seek immediate medical assistance.
The scariest respiratory symptom of all is the shortness of breath that occurs with anaphylactic shock. Anaphylaxis is a sudden reaction to a food allergen. This requires immediate attention, as trouble breathing can quickly become life-threatening.
The following post related to food allergies and asthma – an allergic condition that affects breathing – may be worth a look: Allergies and Asthma: What’s the Link?
General: Excess Fussiness, Sleeplessness or “Colic”
 Every baby cries, but crying continuously and inconsolably for extended periods is unusual. You might hear someone say a baby who cries a lot has colic. Some doctors find colic controversial, but excess crying comes from somewhere, often with insomnia. Doctors also often downplay fussiness, which can delay diagnosing CMA. We hear this from parents all too often!
Every baby cries, but crying continuously and inconsolably for extended periods is unusual. You might hear someone say a baby who cries a lot has colic. Some doctors find colic controversial, but excess crying comes from somewhere, often with insomnia. Doctors also often downplay fussiness, which can delay diagnosing CMA. We hear this from parents all too often!
When should you suspect that crying is excessive (“colic”) and something serious is happening? The going adage is to talk to the doctor if it happens in threes. That is: if your baby cries for 3+ hours in a day, for 3+ days in a week, for over 3 weeks. That can signal gastrointestinal pain, which could result from CMA.
Extreme fussiness can also come with reflux, a rash, or other factors. Keep this in mind when asking your child’s doctor about the possibility of CMA.
General: Low or No Weight Gain or Failure to Thrive (FTT)
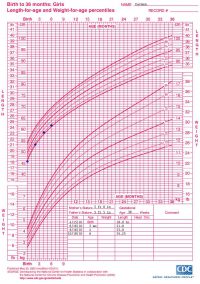 Most infants double their birth weight by six months and triple it by 12 months. Each dot on a growth chart is a percentile. The dots form a growth curve that shows a pattern of growth relative to the population. A child’s head circumference, weight, and height (length, for infants) generally follow a consistent trend over time.
Most infants double their birth weight by six months and triple it by 12 months. Each dot on a growth chart is a percentile. The dots form a growth curve that shows a pattern of growth relative to the population. A child’s head circumference, weight, and height (length, for infants) generally follow a consistent trend over time.
Sometimes though, slow weight gain may lead to a diagnosis of ‘Failure to Thrive’ (FTT), which is one of the symptoms of a cow milk allergy. Slow weight gain is gaining weight more slowly than other children the same age and gender.
Many factors contribute to slow weight gain, and often several factors are at play. Food allergy reactions can cause problems digesting or absorbing food, leading to failure to thrive. For example, babies may not get the nutrition they need because of excessive diarrhea or vomiting. The body may not get all the nutrients needed, which can mean they can’t grow as quickly as they should.
As always, ask your child’s healthcare professional if you are concerned about your child’s weight.
MY BABY HAS ONE OR MORE SYMPTOMS OF A COW MILK ALLERGY
WHAT SHOULD I DO?
Ask the healthcare team! The ideal way they confirm the symptoms of a cow milk allergy is to:
- Remove cow milk from the diet, and
- Re-introduce cow milk, often under a doctor’s supervision.
Many doctors won’t go past step 1 if signs improve. However, step 2 is the best way to confirm a food allergy. If you add cow milk back to the diet and symptoms reappear, CMA can be diagnosed.
Babies allergic with symptoms of a cow milk allergy who require formula need one that’s hypoallergenic, like Neocate® Syneo® Infant. Neocate is safe for babies with food allergies because it contains amino acids, building blocks of protein. Amino acids can’t trigger an allergic reaction the way proteins or peptides in other formulas can. (Read about formula types.)
If you suspect CMA, ask your child’s doctor for a thorough evaluation. Bring this information with you and ask your doctor if your baby might benefit from Neocate. For more on CMA, check out the following resources:
- CMA Symptom Checker
- CMA Guidelines
- The Difference Between CMA and Lactose Intolerance
- Outgrowing CMA






